Sleep apnoea
Sleep apnoea
Sleep apnoea syndrome (SAS, prevalence approximately 5%, more men than women, increases with increasing age) is one of the sleep-related disorders (SRD), more specifically, sleep-related breathing disorders (SRBD).
Compared with healthy sleep, there is a great increase in breathing cessations (AHI = apnoea/hypopnoea index > 10 per hour), in the form of complete apnoea or reductions in airflow (hypopnoea). Central nervous system causes are rarer than the much more common OSA (obstructive sleep apnoea) of local (peripheral) origin. This itself causes central cessations, so mixed forms often occur (approx. 90%). OSAS (obstructive sleep apnoea syndrome) is nearly always associated with heavy snoring that disturbs other sleepers. The interaction of a number of factors, such as supine sleeping position, slack pharyngeal musculature, especially involving the soft palate and uvula and also the hypopharynx (e.g. due to alcohol consumption, sleeping pills), physiological and pathological anatomy (obstructed nasal breathing, enlarged tonsils, macroglossia, obesity) causes temporary complete obstruction of the airways during inspiration.
This causes a drop of about 4% in the blood's oxygen saturation, which is normally 95% to 100% so the oxygen supply to the tissues is impaired. If the episode lasts longer, hypercapnia (a rise in carbon dioxide level) may occur. This then triggers frequent "micro-arousals" via chemosensors, which often do not lead to full awakening; sleep is disturbed with shortened deep sleep phases and an overall reduction in sleep quality with lower relaxation and recovery, which can lead to an increased need for sleep and increased daytime tiredness, daytime somnolence (hypersomnia) and a tendency to fall asleep.
In the long term, apart from quality of life and energy levels, life expectancy is also affected as OSA is associated with high blood pressure, cardiac arrhythmias and depression and there is an increased tendency to stroke, heart attack and accidents.
The diagnosis can be confirmed by recording relevant parameters during sleep at home (cardiorespiratory polygraphy) or in hospital (polysomnography when the patient spends the night in the sleep laboratory); these include ECG, pulse oximetry, EEG, video recording, etc.
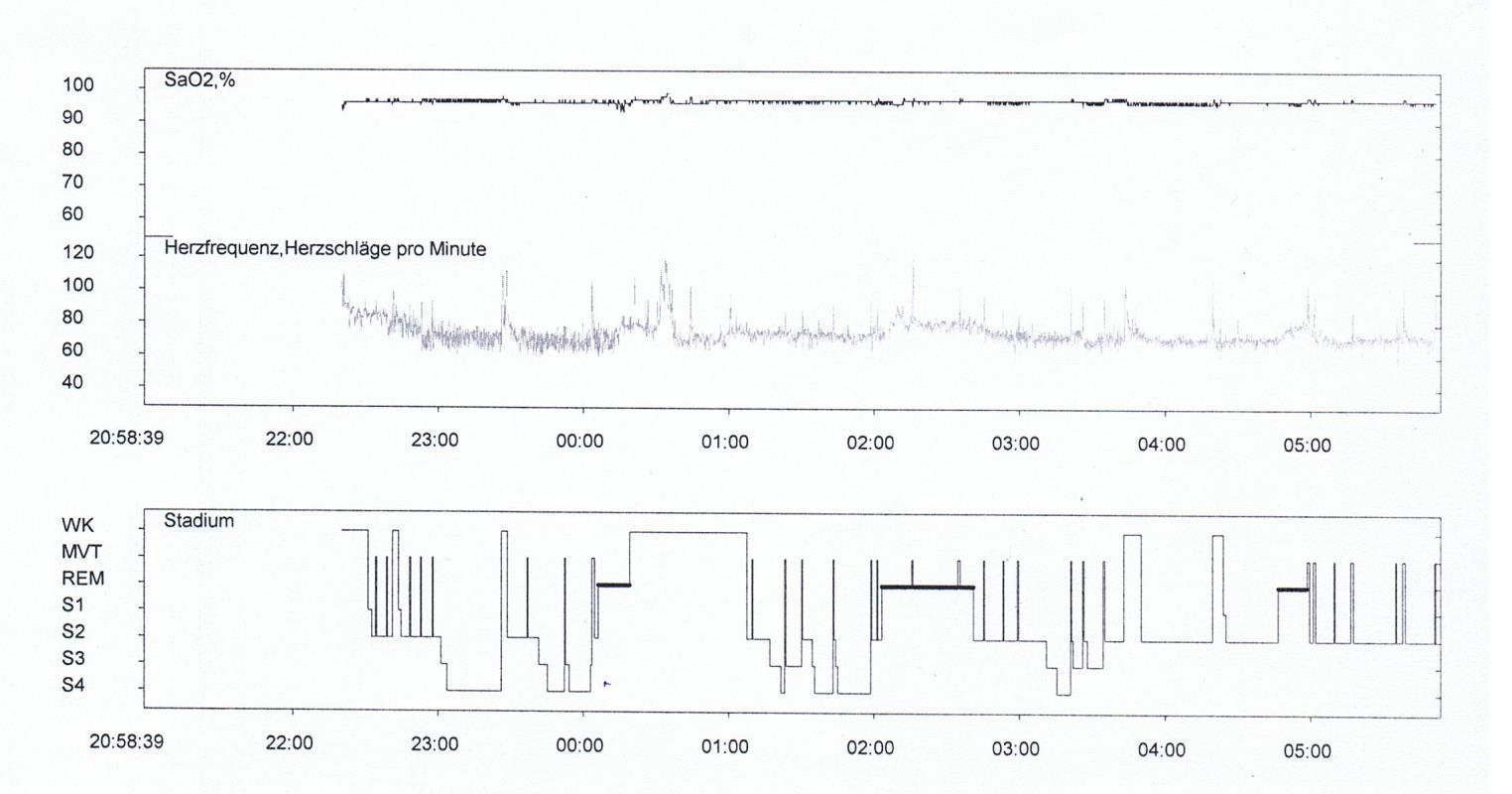 Polysomnogramme with hypnogramme
Polysomnogramme with hypnogramme
Various approaches are used in treatment, alone or in combination:
- Behavioural changes (abstinence from alcohol, lying on the side);
- Removable intraoral devices, usually bimaxillary and usually made in a dental laboratory ("anti-snoring appliance") to move the lower jaw ("protrusion splints") and/or the tongue forward. Thermoformed splints are often made separately for the upper and lower jaw and joined by special metal or plastic joints that allow certain movements.
- "Overpressure" ventilation with pure oxygen and continuous positive airway pressure (CPAP) via a face mask worn during the night.
- Invasive measures in severe cases: surgery to tighten or reduce the volume of tissues.
- Medications, by contrast, have shown little efficacy.
PROBIEREN SIE ES EINFACH AUS !!!
Von uns erhalten Sie professionelle Unterstützung.
Treten Sie mit uns in Kontakt oder nutzen Sie unser Kontaktformular.
Wort des Tages
Schwerpunkttext des Monats
Vergrößernde Optik in der Zahntechnik Vergrößernde Optik in der Zahntechnik |
