Implant
Implants
Dental implants are synthetic structures for insertion into the bone and are normally similar in shape to the root of a tooth (cylindrical or conical). They are mainly used for intraoral anchorage of fixed or removable restorations (superstructure). In special cases they are also used for anchorage of orthodontic appliances or maxillofacial prostheses (epitheses).
Implants in the 21st century are rarely made from zirconium dioxide. In the majority of cases they are made from pure titanium. This light and stable metal is bioinert, apposition and deposition of bone is therefore possible. Rigid fixation of the implant by gap-free, bone growth on the surface, i.e. osseointegration, is vitally important for ensuring permanent stability during functional loading of implants. Suitable procedures for roughening, creating niches and increasing the surface area facilitate migration of living bone cells and ingrowth of bone into the implant surface. This also applies for the neck of the implant which, only during the very early stages of development, was finished to a smooth polished surface.
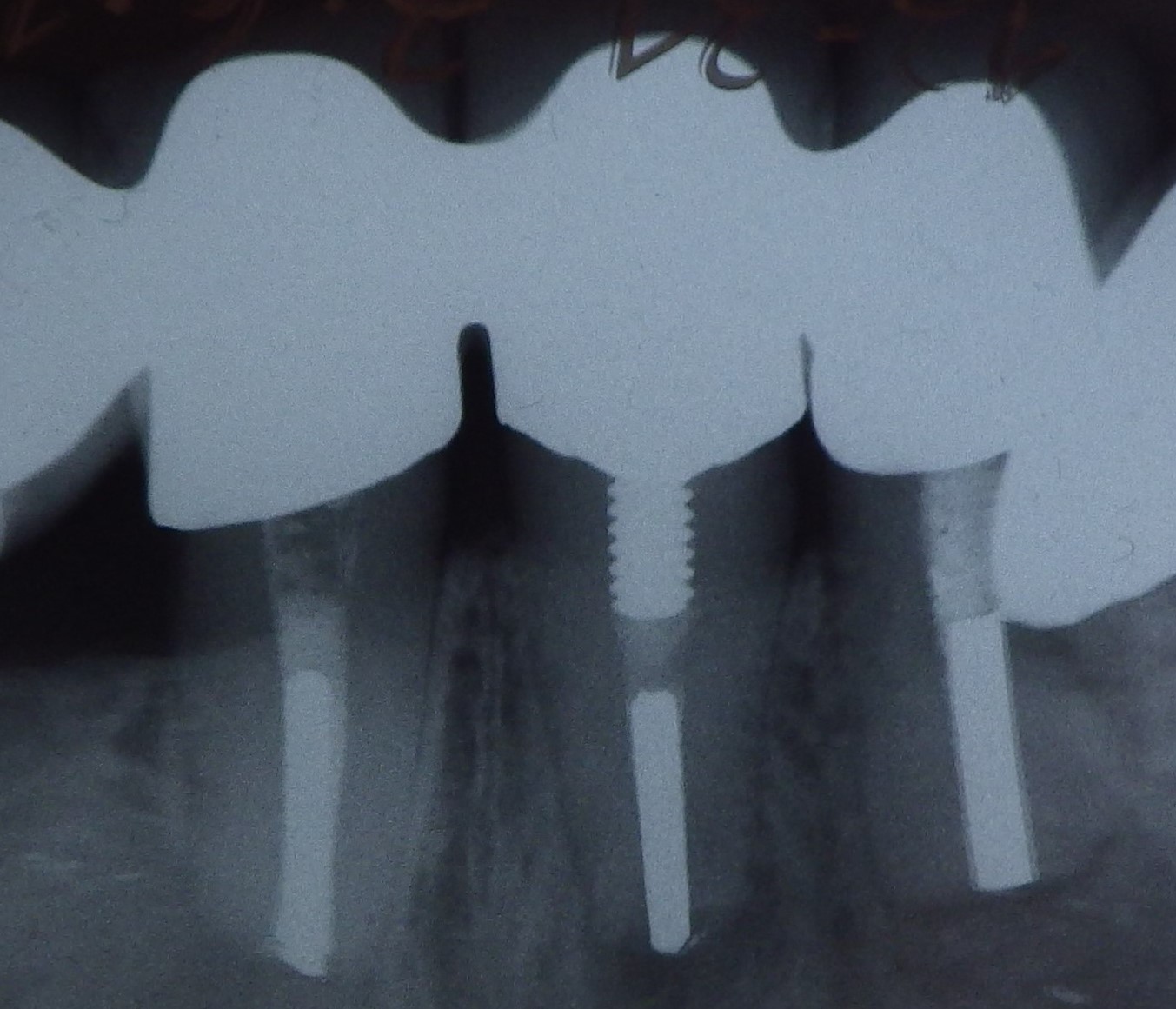
To prepare for implant placement, a narrow hole is first drilled in the bone, which is then widened incrementally using other drills (mainly in compact bone) and/ or bone condensing instruments (mainly in cancellous bone) in ascending diameter until the planned final diameter of the bone cavity is achieved. Manual or mechanical placement of the cylindrical-conical implant with external thread(s) is the same type of procedure as controlled insertion of a screw. Adequate primary stability can often be achieved by a slight press fit and self-tapping thread.
The upper edge of the implant, i.e. the platform, can be placed at bone or tissue level.
 Titanium implants at bone level
Titanium implants at bone level
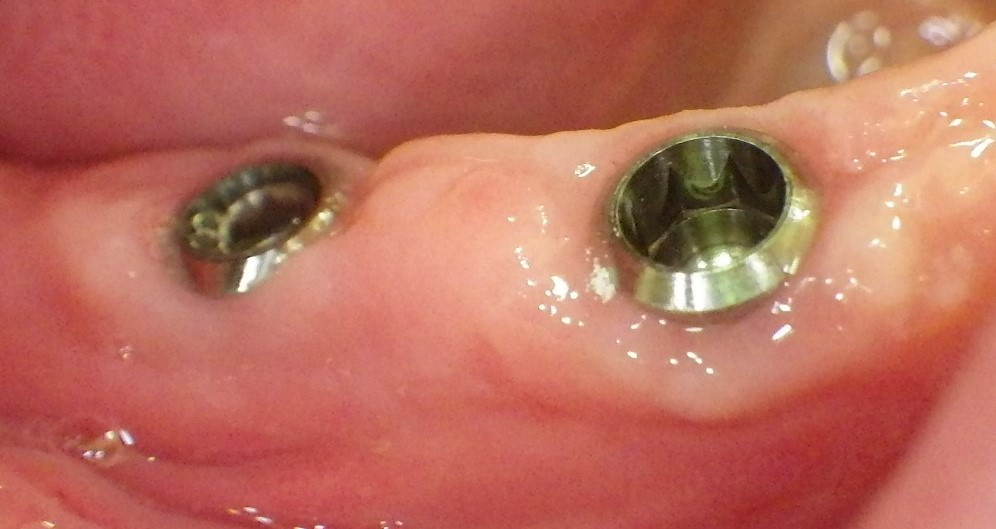 Implants at tissue level
Implants at tissue level
Healing may be submerged (under the densely sealed mucosa covering) or open (using intraoperative forming of a gingival collar).
There is often less bone volume available for implants due to bone resorption after tooth loss. Bone augmentation procedures are then used (e.g. GBR, guided bone regeneration) or smaller (e.g. reduced diameter) implants placed. Standard implants have a platform diameter of approx. 4 mm. The term for platform sizes that are much larger than this is "wide"; the term for much smaller platform sizes is "narrow" and even thinner implants are known as "mini-implants".
Modern dental implants are usually two-part. The implant (tooth root replacement) and abutment (core unit) have an interlocking and frictional connection. The internal conical connection with additional interlocking "tongue and groove" elements for providing rotational security has become the established design. Retention screws are tightened using defined torque to exclude the risk of movements, loosening and material overloading.
 A modern implant
A modern implant
Though previously the fitting surface of the abutment always had the same diameter as the implant platform, modern abutments are often smaller in this region. This so-called "platform switching" is intended to improve bone preservation.
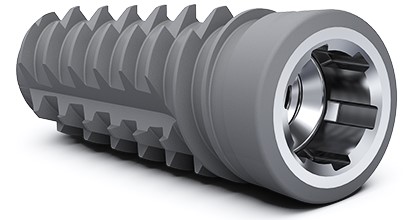 A latest generation implant
A latest generation implant
It is important to strive for as correct an anatomical emergence profile as possible to ensure the natural appearance of implant-supported restorations (red-white aesthetics) and healthy peri-implant conditions.
Want to give it a try ...
... or need professional advice?
Get in touch with us or click Contact.
Word of the day
| English | German |
|---|---|
| non-keratinized | nichtkeratinisiert |
Focus text of the month
Root canal posts are inserted centrally into adequately long, straight sections of devitalised, root-filled teeth which show no pathological findings either clinically or radiologically. Severe vertical and horizontal structure loss from the clinical crown is an indication… Root canal posts are inserted centrally into adequately long, straight sections of devitalised, root-filled teeth which show no pathological findings either clinically or radiologically. Severe vertical and horizontal structure loss from the clinical crown is an indication for root canal posts. The preferred method is generally to insert the root canal post, so that it (by predrilling with ascending diameters) virtually fills the prepared post site and fits close to the dentine wall. That section of the root canal post in the root should be at least as long as the crown restoration, leaving a few millimetres of the root canal filling to seal the apex. Isolated concepts have also been developed with smooth metal posts projecting apically beyond the tooth and intended for anchoring in the bone (transdental fixation).
Restoration with a temporary post is seldom practical due to the increased fracture and reinfection rate; a definitive root canal post should be inserted as early as possible.
Customised root canal posts (often made from precious metal alloys), cast after waxing up directly in the root canal or indirectly after taking an impression of the root canal lumen (using burnout posts), can also be used for filling lumina with oval or irregular cross sections, as well as two or three divergent canals each fitted with a post inserted, if necessary, through the opening of another canal. The core build-up(s), or even the entire crown (historically: post crown) can be integrated. |

 Three different root canal posts
Three different root canal posts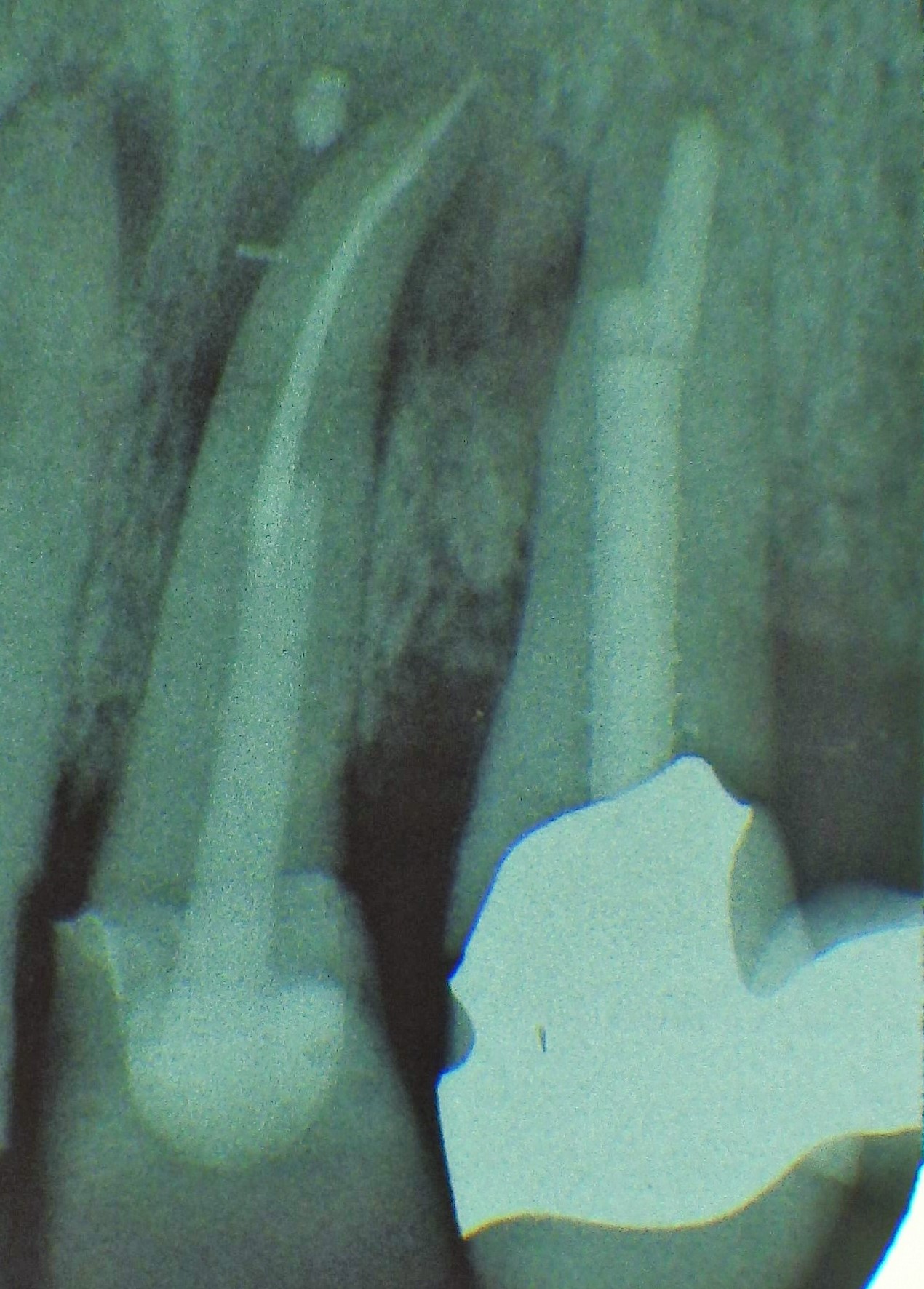 Tooth 14 conical and smooth, tooth 13 cylindrical and threaded
Tooth 14 conical and smooth, tooth 13 cylindrical and threaded