Dental polishers
Dental Polishers
In dentistry and dental technology very different materials require smoothing and polishing. This ranges from exceptionally hard natural tooth enamel to the surfaces of filling materials (composites, compomers or amalgam), fixed restorations (metal alloys or ceramics), implant components (titanium, other metals or zirconia), appliances, splints or dentures (all types of hard and soft materials).
The dental polishers used in standard handpieces are rotary instruments with a metal or plastic shank. The smoothing and polishing section of the instrument is attached to the shank – whether rigidly connected or via press-on, clamp or screw connection (e.g. with mandrels). Some polishers are not active themselves and require the additional use of polishing pastes as consumable materials (in particular for prophylaxis).
Easy, clean results are produced with all other polishers. In this case the working section is made of rubber or silicone. Abrasive materials (e.g., silicon carbide or corundum and mainly diamonds are used for very hard materials, in particular ceramics) of a suitable, selected grit size are embedded in the surface or impregnate the entire working section.
A wide range of polisher shapes is available for different applications. Typical shapes are points, cups and discs for the dental practice and wheels, cylinders/arbor bands and torpedoes for the dental laboratory.
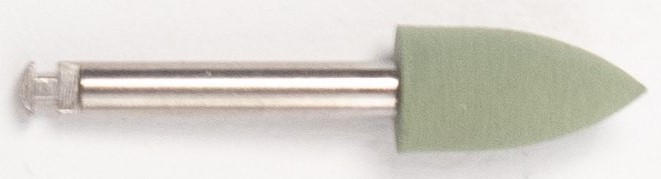 A dental polisher
A dental polisher
Surfaces of materials are smoothed and polished in one or more working stages. Technically, the individual processing stages vary either in the different pressure applied and/or motor speed but mainly by using abrasives/polishers with different degrees of hardness and grit sizes (specific for each stage). Polishing techniques often differentiate between two-step pre-polishing (coarse polish) and high-lustre polishing (fine polish), depending on the material, initial condition, required final state and up to three steps. The first/coarsest step is frequently a transition from preparing/contouring; at this stage significant (macroscopic) amounts of material are still removed. In the subsequent steps the main focus of the work is more on reducing (increasingly microscopic) surface irregularities (surface roughness). The final step produces a smooth surface, in general with a silky sheen or high-lustre/shining finish. Often the different colours of the polishers facilitate the assignment of specific instruments to the respective working stages. All diamond grit polishers have uniformly standardised coloured rings for identifying the different fineness of each polishing step.
To rule out cross contamination between patients in clinical dental medical applications, preference should be given to polishers, which are either suitable for sterilisation in an autoclave to ensure safe multiple use or which are designed as single-use products from the outset (use for one single patient only).
Want to give it a try ...
... or need professional advice?
Get in touch with us or click Contact.
Word of the day
| English | German |
|---|---|
| plaster solvent | Gipsauslöser, Gipsentferner, Gipslösebad, Gipslösemittel, Gipslöser |
Focus text of the month
Root canal posts are inserted centrally into adequately long, straight sections of devitalised, root-filled teeth which show no pathological findings either clinically or radiologically. Severe vertical and horizontal structure loss from the clinical crown is an indication… Root canal posts are inserted centrally into adequately long, straight sections of devitalised, root-filled teeth which show no pathological findings either clinically or radiologically. Severe vertical and horizontal structure loss from the clinical crown is an indication for root canal posts. The preferred method is generally to insert the root canal post, so that it (by predrilling with ascending diameters) virtually fills the prepared post site and fits close to the dentine wall. That section of the root canal post in the root should be at least as long as the crown restoration, leaving a few millimetres of the root canal filling to seal the apex. Isolated concepts have also been developed with smooth metal posts projecting apically beyond the tooth and intended for anchoring in the bone (transdental fixation).
Restoration with a temporary post is seldom practical due to the increased fracture and reinfection rate; a definitive root canal post should be inserted as early as possible.
Customised root canal posts (often made from precious metal alloys), cast after waxing up directly in the root canal or indirectly after taking an impression of the root canal lumen (using burnout posts), can also be used for filling lumina with oval or irregular cross sections, as well as two or three divergent canals each fitted with a post inserted, if necessary, through the opening of another canal. The core build-up(s), or even the entire crown (historically: post crown) can be integrated. |

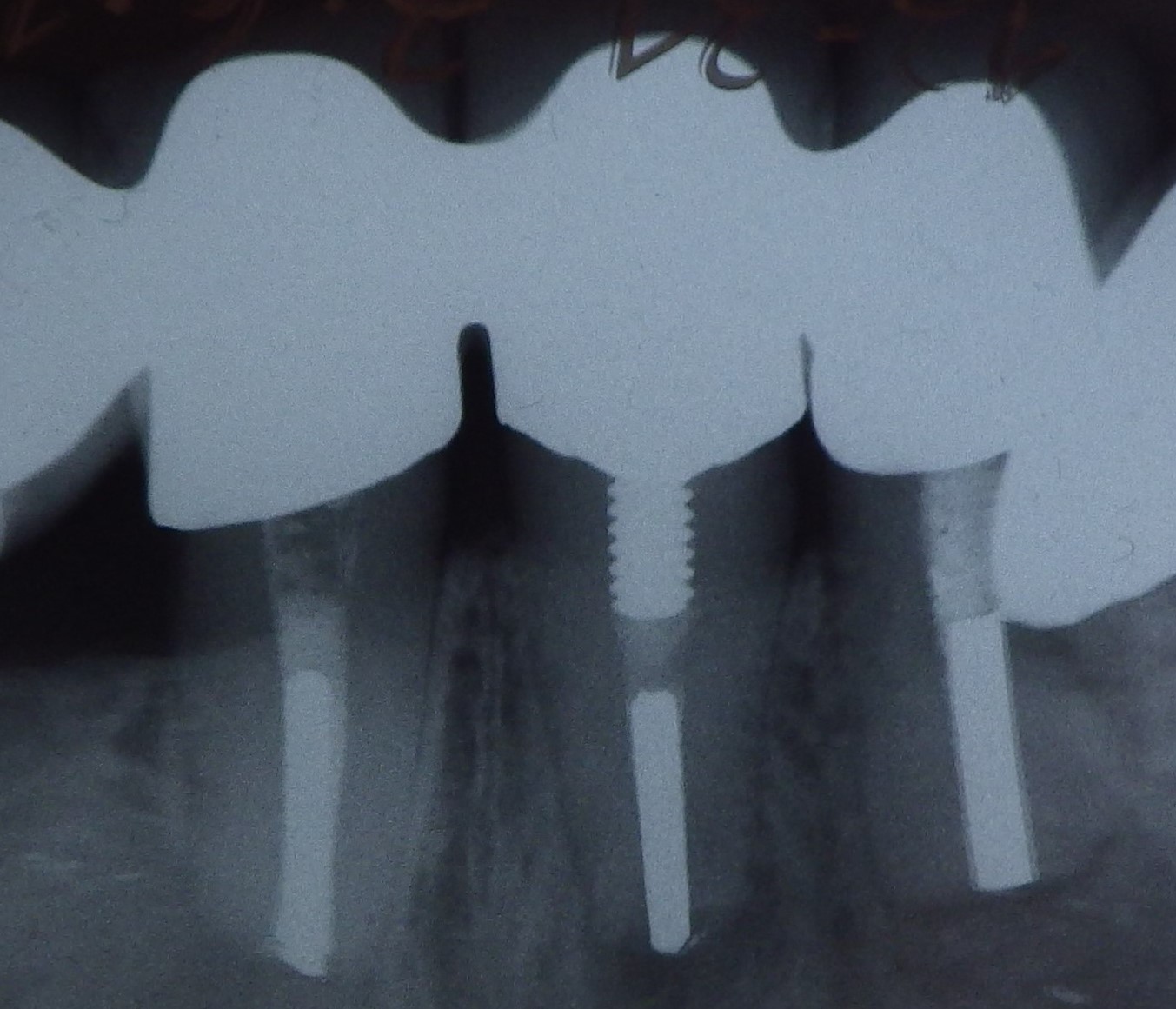 Three different root canal posts
Three different root canal posts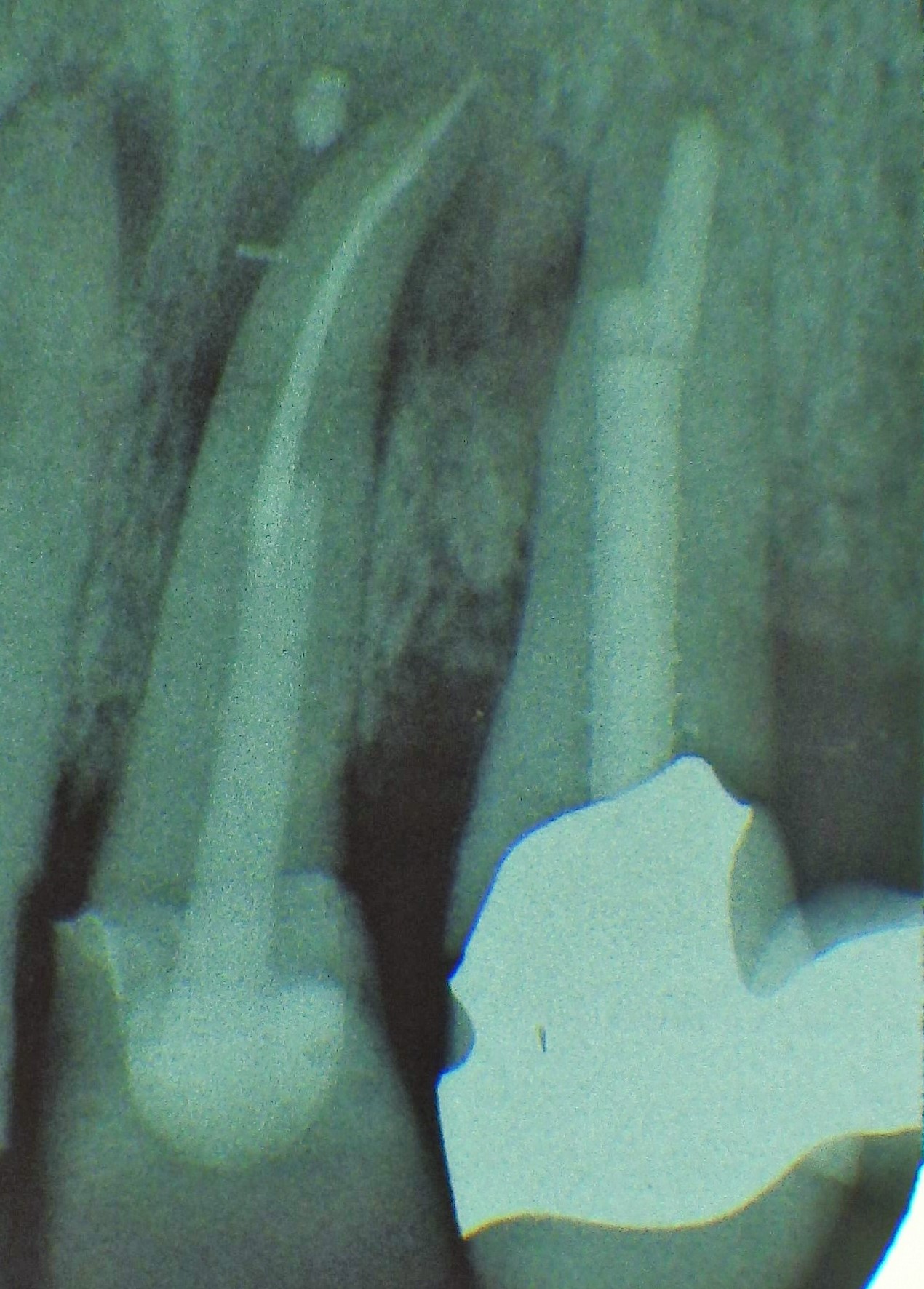 Tooth 14 conical and smooth, tooth 13 cylindrical and threaded
Tooth 14 conical and smooth, tooth 13 cylindrical and threaded