Bone augmentation
Bone augmentation
Targeted build-up of tissue is referred to as augmentation.
The aim of bone augmentation procedures in dentistry is, on the one hand, the reconstruction of lost bony substance, e.g. in the case of periodontal defects (filling of intrabony pockets) or atrophy of the alveolar ridge and, on the other hand, gaining additional bone volume in areas previously without bone, e.g. in the extraction socket (socket preservation) or at the sinus floor (sinus floor augmentation).
Generally, additional (resorbable or non-resorbable) materials are used for augmentation:
This may involve membranes, which are mainly used for protecting the augmentation area against ingrowing mucosa and connective tissue (guided bone regeneration, GBR). Most granulated bone augmentation materials can be synthetic in origin; animal materials are frequently bovine (i.e. cattle) bone. Natural bone often provides crucial structural benefits compared with synthetic materials, such as very high porosity, which facilitates storage of tissue fluids and penetration of newly formed autogenous bone.
In the case of human bone a differentiation is made between autografting (donor is recipient), involving removal of bone from other regions of the jaw or body, and allografting (donor ≠ recipient), i.e. from cadaver bone.
Any foreign tissue must be very thoroughly cleaned of viable tissue (sterilisation, denaturation of proteins, removal of organic components etc.) to exclude the risk of infection.
Some augmentation procedures require a second intervention in a different region and/or at a different time, e.g. to harvest graft material or remove non-resorbable materials or auxiliary devices.
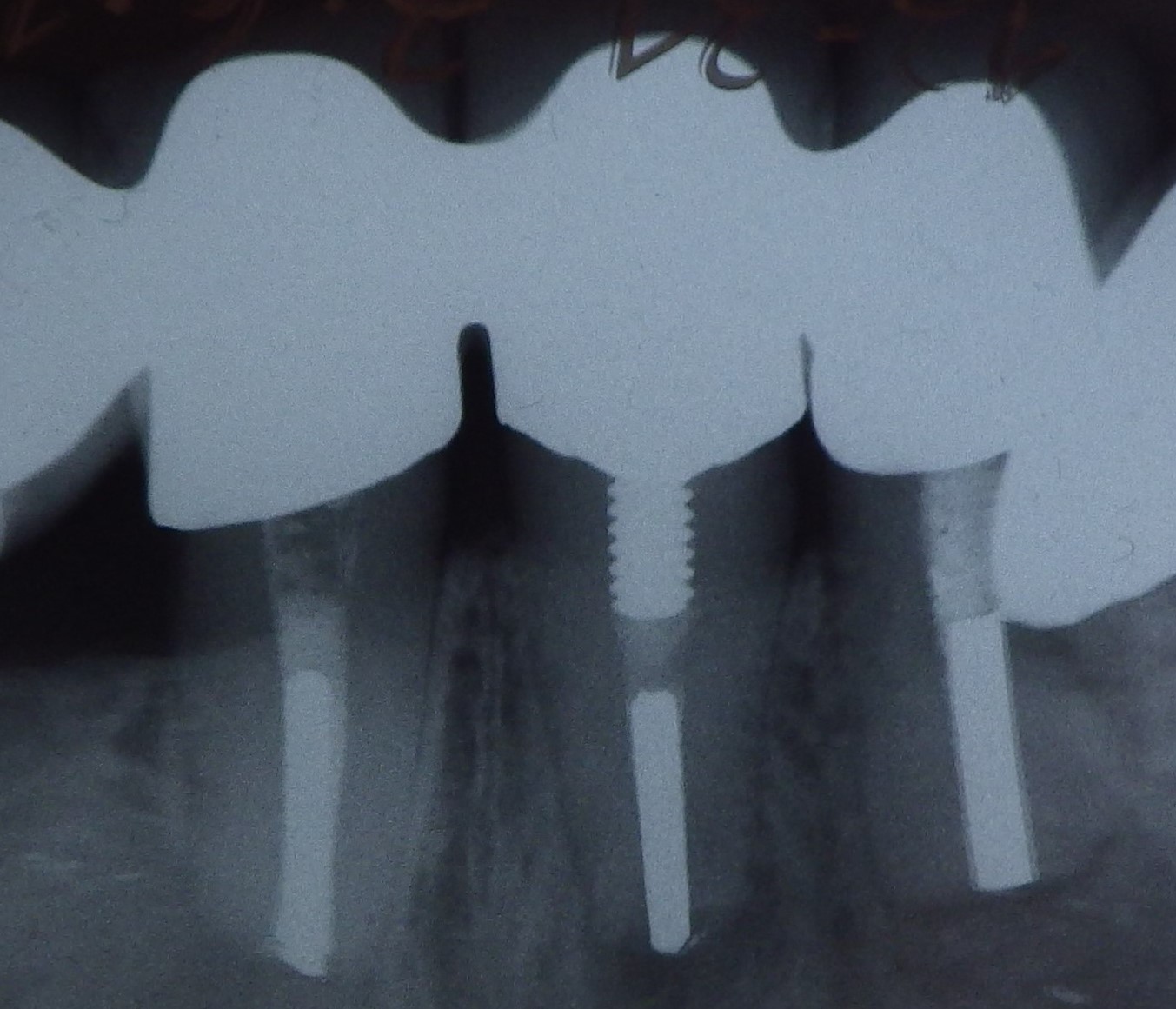
Bone augmentation procedures are often used to prepare for or accompany implant placement to achieve an aesthetic and functionally optimal implant position. In addition to distraction osteogenesis, the gold standard is augmentation using autologous bone in the form of collected bone chips mixed with autologous blood; recently also using bone cells cultivated in a tissue culture (bone tissue engineering), above all in the form of an autologous block graft.
Bone blocks extracted from other regions are secured in position at the required implant site using membranes, pins, screws etc. Typical areas for bone augmentation in the form of an onlay graft are the posterior region of the mandible (compensation of alveolar ridge atrophy) and the anterior region of the maxilla (reinforcing the labial bone lamella).
The anticipated loss of volume of the graft of up to 50% during the healing phase can be compensated for by initially increasing the size of the graft.
While autologous bone heals completely, osteoconductive or osteoinductive foreign materials can often be resorbed only partially and very slowly and remain detectable even after many years.
The success of augmentation can be promoted by the use of growth factors (mainly proteins, hormones), which stimulate bone growth (e.g. BMPs = bone morphogenetic proteins).
Want to give it a try ...
... or need professional advice?
Get in touch with us or click Contact.
Word of the day
| English | German |
|---|---|
| auscultation | Auskultation |
Focus text of the month
Root canal posts are inserted centrally into adequately long, straight sections of devitalised, root-filled teeth which show no pathological findings either clinically or radiologically. Severe vertical and horizontal structure loss from the clinical crown is an indication… Root canal posts are inserted centrally into adequately long, straight sections of devitalised, root-filled teeth which show no pathological findings either clinically or radiologically. Severe vertical and horizontal structure loss from the clinical crown is an indication for root canal posts. The preferred method is generally to insert the root canal post, so that it (by predrilling with ascending diameters) virtually fills the prepared post site and fits close to the dentine wall. That section of the root canal post in the root should be at least as long as the crown restoration, leaving a few millimetres of the root canal filling to seal the apex. Isolated concepts have also been developed with smooth metal posts projecting apically beyond the tooth and intended for anchoring in the bone (transdental fixation).
Restoration with a temporary post is seldom practical due to the increased fracture and reinfection rate; a definitive root canal post should be inserted as early as possible.
Customised root canal posts (often made from precious metal alloys), cast after waxing up directly in the root canal or indirectly after taking an impression of the root canal lumen (using burnout posts), can also be used for filling lumina with oval or irregular cross sections, as well as two or three divergent canals each fitted with a post inserted, if necessary, through the opening of another canal. The core build-up(s), or even the entire crown (historically: post crown) can be integrated. |

 Three different root canal posts
Three different root canal posts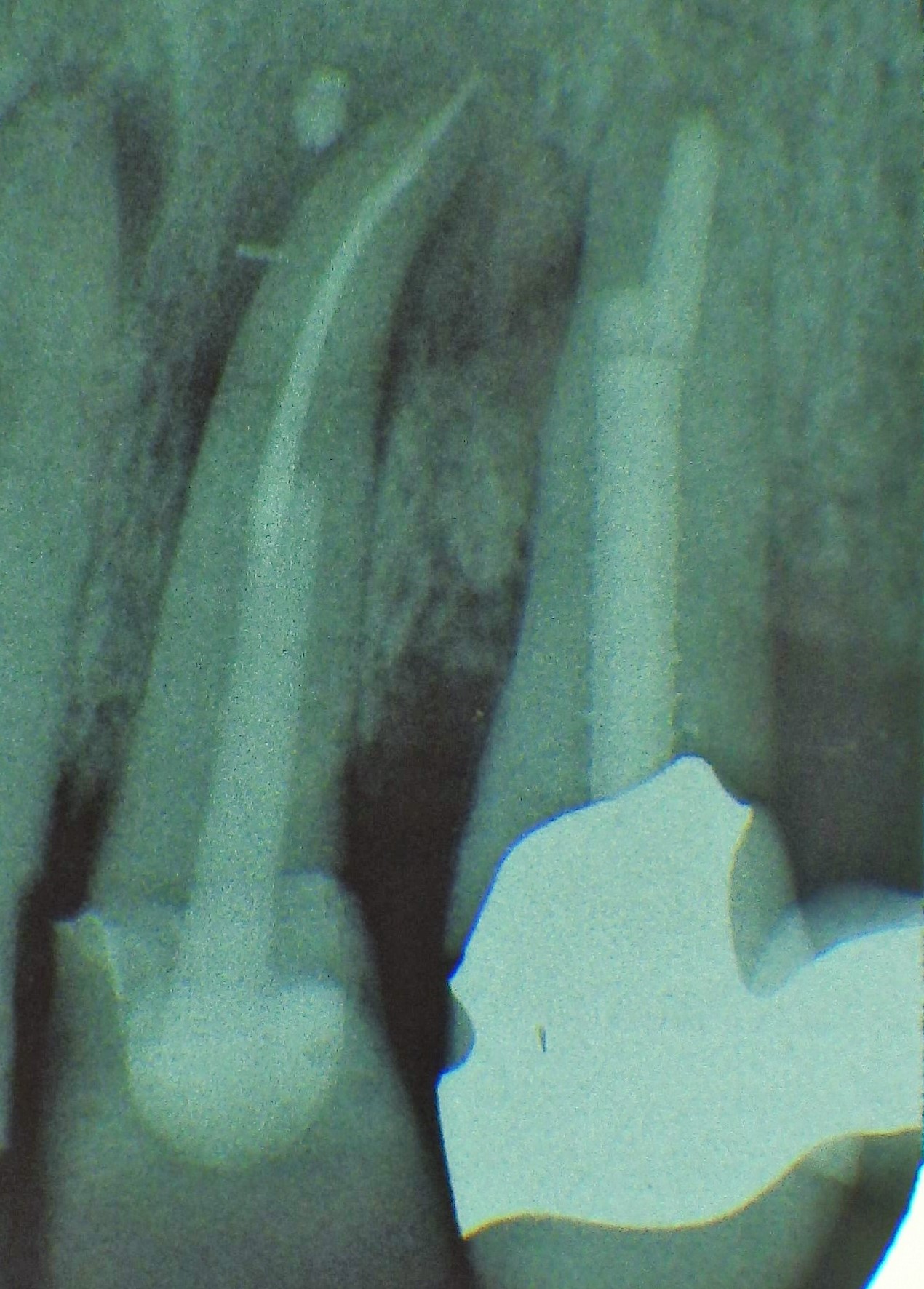 Tooth 14 conical and smooth, tooth 13 cylindrical and threaded
Tooth 14 conical and smooth, tooth 13 cylindrical and threaded